Publié le 09 December 2024
Why does my hip prosthesis hurt ?
Why can a hip prosthesis be painful ? It is important to differentiate between persistent pain since the operation and pain that arises after several years of good joint function. When pain occurs immediately after surgery and does not go away, several causes can be considered. Infectious issues The likelihood of infection (bacteria developing around the […]
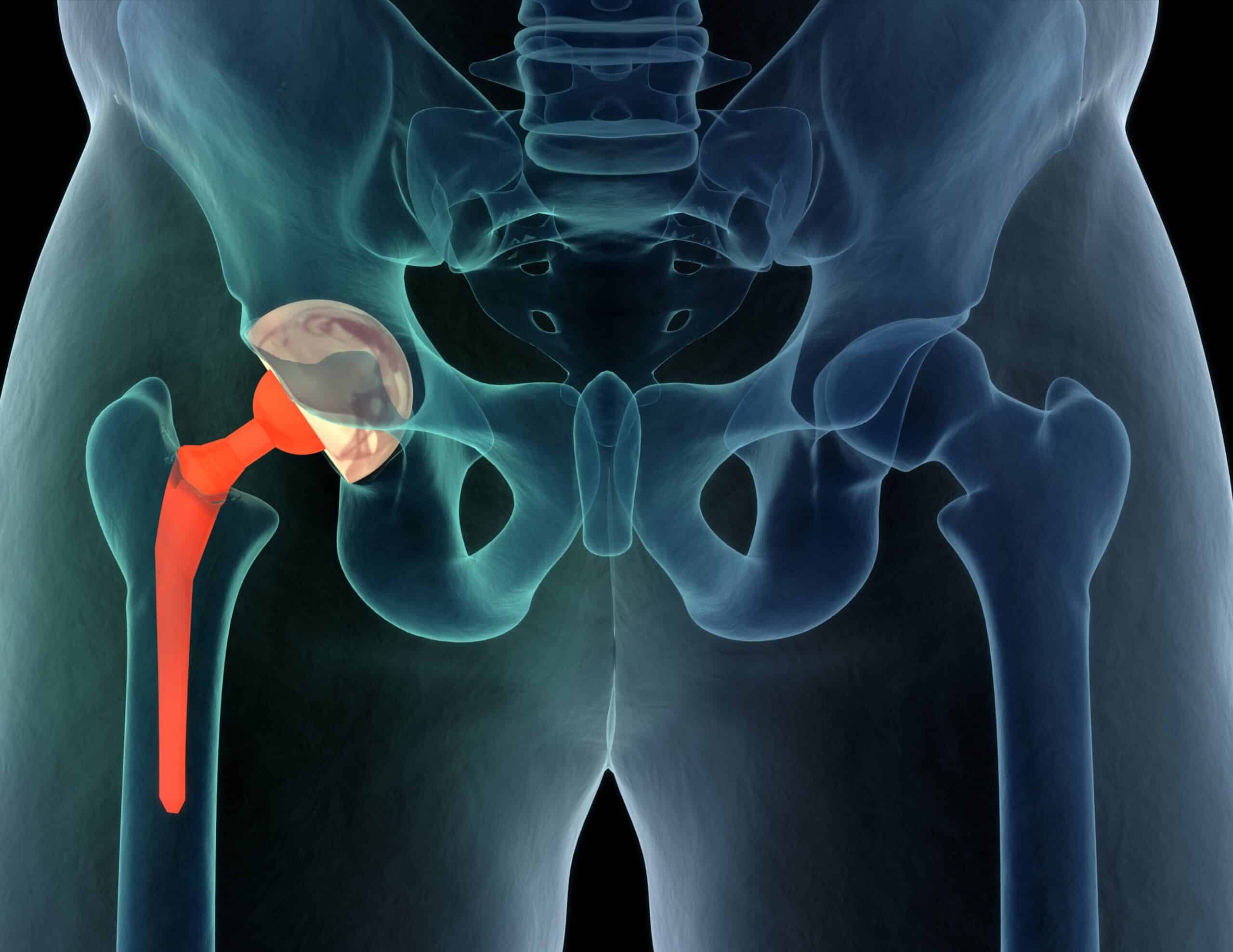
Why can a hip prosthesis be painful ?
It is important to differentiate between persistent pain since the operation and pain that arises after several years of good joint function.
When pain occurs immediately after surgery and does not go away, several causes can be considered.
Infectious issues
The likelihood of infection (bacteria developing around the prosthesis) following the implantation of a prosthesis is low (0.5% to 1% of cases), but it is a serious complication.
Some infections are obvious (fever, discharge at the scar, inflammation), but certain bacteria can develop slowly, manifesting only as pain or joint discomfort. Persistent pain after prosthetic implantation should always raise suspicion of infection, and certain tests (blood tests, X-rays, joint fluid aspiration) can help diagnose it. Diagnosing an infection can sometimes be challenging.
Bone integration problems
The stability of the implants in the bone is crucial for a successful outcome. A prosthesis that does not firmly integrate into the bone will exhibit abnormal mobility, causing pain during activity and walking. A delayed bone integration is possible and might resolve spontaneously, but after 6 to 12 months of monitoring, non-integration of the prosthesis should be suspected. Appropriate tests include X-rays, CT scans, or even bone scintigraphy to assess implant integration.
Mechanical issues
Improper sizing or positioning of the implants (joint length, component orientation, muscle tension adjustment, etc.) can result in joint kinematics abnormalities. This can lead to conflicts between metallic components, instability, or excessive/insufficient tension in tendons or muscles, causing pain and abnormal mechanical sensations.
A 3D CT scan can provide precise measurements of the joint. In our team, we particularly recommend preoperative 3D imaging to ensure proper geometric reconstruction of the joint.
Tendinous pain
Tendonitis around the hip (e.g., gluteal, psoas muscles) may occur independently of the prosthesis placement but can sometimes be caused by improper prosthesis positioning. For example, a cup that extends beyond the pelvic bone frame can cause psoas tendonitis, while excessive lengthening of the joint can affect the gluteus medius muscle. Rigorous analysis of joint geometry in 3D can confirm proper reconstruction, and exams like ultrasounds can detect tendinopathy.
Referred pain
The hip is a deep joint at the crossroads of many anatomical structures (nerves, tendons, blood vessels). Sometimes referred pain originating from the spine (sciatica, cruralgia) or the abdomen (hernias, digestive issues) can mimic hip pain without being related to the joint or the prosthesis. A thorough physical examination, supplemented by additional tests if needed, can confirm these diagnoses.
Misdiagnosis
When the prosthesis operation does not alleviate pre-existing pain, the absence of a link between the pain and the joint condition that led to the operation should be considered. This is especially relevant for young patients and/or those with mild to moderate joint degeneration. For these patients, a careful and thorough diagnostic approach is essential before deciding on surgery. Additional tests (CT scan, MRI) or therapeutic trials (injections) may be helpful.
Finally, when pain appears years after the prosthesis implantation following a period of good results, prosthesis wear (particularly for prostheses with polyethylene components), early loosening (loss of bone anchorage), or infection should be suspected. Simple exams and X-rays usually suffice for diagnosis.
When should you consult for a painful hip prosthesis ?
In the weeks or months following prosthesis placement, the presence of pain does not necessarily indicate complications, but regular follow-up with the surgeon is prudent until the pain subsides. Progressive improvement is reassuring. Conversely, stagnation or worsening of pain should prompt the patient to see their surgeon earlier.
In cases of late-onset pain that does not resolve after a few weeks, it is advisable to consult the surgeon who performed the prosthesis implantation. In all cases, spaced but regular monitoring of all hip prostheses is recommended.
What treatments are available for a painful hip prosthesis ?
The variety of causes that can explain pain around a hip prosthesis means there are different treatments available.
Some pain can be treated with simple measures (rehabilitation, manual therapy), especially when the problem is not related to a prosthesis placement issue.
In some cases, injections may be recommended for tendon pain or inflammation.
Revision surgery is suggested in cases of significant mechanical issues, proven infection, or lack of bone integration. Significant prosthesis wear or bone lesions related to wear may also necessitate surgical intervention. Surgery may involve partial or total prosthesis replacement, and in some cases, more complex procedures (bone grafts, tendon interventions, custom prostheses, or reconstructions).
In any case, decisions about interventions on an existing prosthesis require significant expertise, a rigorous approach, and the use of modern diagnostic tools (particularly 3D CT scans).
What tools help reduce the risk of complications ?
First, the surgeon’s experience with hip prostheses is critical for achieving reliable and reproducible results. A well-conducted diagnostic approach, clear preoperative explanations, and the use of 3D planning tools (CT scans) are key to achieving a good outcome.
Finally, in our experience, the use of customized hip prostheses, designed and manufactured based on each patient’s morphology, optimizes the result quality. The anterior hip approach, which respects the musculature without cutting tendons or muscles, is also advantageous for optimized anatomical recovery.